
『蛋白粉傷腎』是沒有科學依據的,屬於未經證實的謠言。因為蛋白質並不由腎臟排泄,腎臟排出的是尿素;而尿素是一種極易排出的小分子,排泄不產生負擔 一、 蛋白粉/蛋白質不經腎臟排泄
現在網上有些人張口就是「蛋白粉傷腎」、「增加腎臟負擔」之類的話。

我搞不懂的是,這都2022年了,怎麽還會有這種觀點呢?生理學告訴我們, 腎不會排出膳食蛋白質,腎排泄的是尿素:
這其實在我們之前的文章中解釋過:
用圖形表示,就是這樣的:
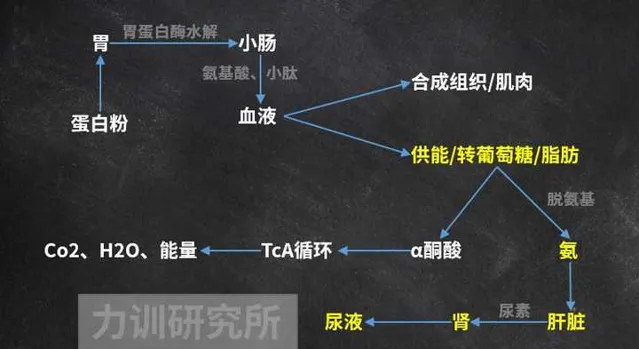
也就是說,吃下去的蛋白質,只有 部份 用於供能,最後代謝為二氧化碳、水和尿素,後者從腎臟排出,哪來的蛋白質讓腎臟過濾/排泄?以我對杠精的了解,它們又會編:「排出尿素也會增加腎臟負擔」,所以我們接下來講講尿素。
二、尿素排泄對腎臟有負擔嗎?
尿素是一種無色無味的中性分極小子,總體上不影響血液酸堿性 [9] [10] [11] 。
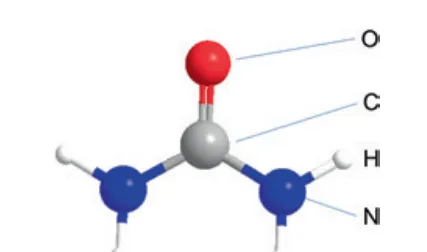
尿素分子分非常小,具有很高水溶性的 [12] ,極易隨體液排出體外。除了尿液,人類還透過汗液 [13] 、眼淚 [14] 、唾液 [15] [16] 和糞便 [17] [18] [19] 排出尿素。
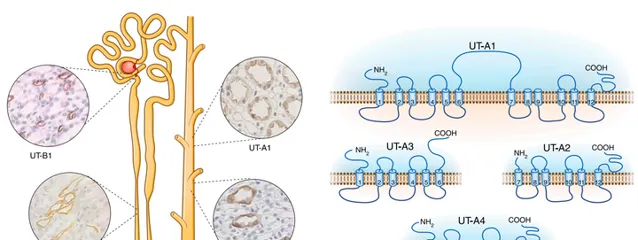
註意, 尿素太容易排出體外,人反而要努力留住它, 因為它能調節滲透壓,留下尿素可以留下很多水分,減少水分排泄,濃縮尿液 [20] [21] [22] [23] ,從而幫助我們生存;人挽留尿素靠尿素轉運蛋白Urea Transporter ,簡稱UT。
UT有A、B等大類 [24] ,在腎臟、心臟、腦、睪丸、泌尿系統等組織中有較廣泛的分布。UT-B在大腦中大量存在,因為大腦中也含有較多尿素 [25] [26] 。UT-A又分了多種,有A1、A2、A3等。UT-A1一般分布在腎髓內集合管(IMCD)細胞的頂端膜上,它們能我們快速吸收尿素。
尿素多了,滲透壓上升,水分被回收 [27] [28] 、尿液濃縮。這在演化上也說得通,因為水是寶貴的生存資源。
不僅人類,許多其他哺乳動物也是如此,Bankir等人使用有基因特征的小鼠模型進行研究 [29] ,它們體內不能產生尿素轉運蛋白B(UT-B)。進食高蛋白食物後,正常小鼠血液尿素水平提高了44%,而UTB缺陷小鼠的尿素濃度沒有增加
為啥沒增加?排泄出去了。
隨飲食中蛋白質的比例從10%增加到40%,UT-B基因缺陷小鼠的尿素排泄量增加了 5倍 。多項類似研究也得到了類似結果 [30] [31] [32] ,支持Bankir等人的結論,證明了尿素具有「易排泄,難保留」的特性。
因此『腎臟排泄尿素有壓力』,又是憑空編造的謠言。
三、乳制品蛋白能降低腎結石機率
有許多大型研究支持這樣的觀點,即乳制品蛋白質能降低腎結石發病率。
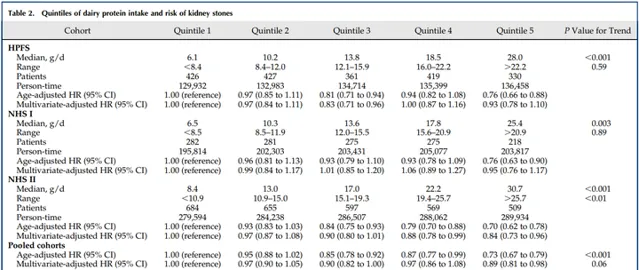
例如Pietro等人 [33] 對健康專業人員研究(42919人)、美國護士健康研究I(60128人)和護士健康研究II(90629人)的數據進行了分析,攝入奶制品蛋白導致結石風險降低26%。
註意,如果多攝入非乳制品動物蛋白,男性患腎結石的風險顯著升高。
也就是說,乳制品和乳清蛋白粉與肉類的健康效果存在差異,肉類可能對腎結石有促進作用,而乳制品和乳清蛋白粉可能對腎結石有一定程度的保護作用。
擴充套件閱讀
肉崽:力訓研究所課程介紹
不健身直接吃蛋白粉會怎麽樣?
為什麽減脂容易掉肌肉?
當代年輕人為什麽尿酸會高?
參考
- ^ a b Brosnan, J.T. Interorgan amino acid transport and its regulation. J. Nutr.133:2068S2072S, 2003.
- ^ Jungas, R.L, M.L. Halperin, and J.T. Brosnan. Qualitative analysis of amino acid oxidation and related gluconeogenesis in humans. Physiol. Rev. 72:419-448, 1992.
- ^ Havir EA, Tamir H, Ratner S, Warner RC (1965) Biosynthesis of urea XI. Preparation and properties of crystalline argininosuccinase. J Biol Chem 240:3079–3088
- ^ Hoberman HD, Havir EA, Rochovansky O, Ratner S (1964) Biosynthesis of urea X. Stereospecificity of the argininosuccinase reaction. J Biol Chem 239:3818–3820
- ^ Dimski DS (1994) Ammonia metabolism and the urea cycle: function and clinical implications.J Vet Intern Med 8:73–78
- ^ Meijer AJ, Lamers WH, Chamuleau R (1990) Nitrogen metabolism and ornithine cycle function. Physiol Rev 70:701–748
- ^ Lusty C, Ratner S (1972) Biosynthesis of urea XIV. The quaternary structure of argininosuccinase. J Biol Chem 247:7010–7022
- ^ Petrack B, Ratner S (1958) Biosynthesis of urea VII. Reversible formation of argininosuccinic acid. J Biol Chem 233:1494–1500
- ^ Bjerrum K, Vilstrup H, Almdal T, Ostergaard L (1990) No effect of bicarbonate-induced alkalosis on urea synthesis in normal man. Scand J Clin Lab Invest 50:137–141
- ^ Boon L, Blommaart PJ, Meijer AJ, Lamers WH, Schoolwerth A (1994) Acute acidosis inhibits liver amino acid transport: no primary role for the urea cycle in acid–base balance. Am J Physiol Renal Physiol 267:F1015–F1020.
- ^ Boon L, Blommaart PJ, Meijer AJ, Lamers WH, Schoolwerth AC (1996) Response of hepatic amino acid consumption to chronic metabolic acidosis. Am J Physiol271:F198–F202
- ^ Fenton R. A. (2008). Urea transporters and renal function: lessons from knockout mice. Curr. Opin. Nephrol. Hypertens. 17, 513–51810.
- ^ Schwartz IL, Thaysen JH, Dole VP (1953) Urea excretion in human sweat as a tracer for movement of water within the secreting gland. J Exp Med 97:429–437
- ^ Thaysen JH, Thorn NA (1954) Excretion of urea, sodium, potassium and chloride in human tears. Am J Physiol 178:160–164
- ^ Albrectsen SR, Thaysen JH (1955) The excretion of urea by the human parotid gland. Scand J Clin Lab Invest 7:231–238
- ^ Carco P, Canciullo D (1958) Urea excretion through the human salivary glands. Ann Otol Rhinol Laryngol 67:1050–1065
- ^ Bliss DZ, Stein TP, Schleifer CR, Settle RG (1996) Supplementation with gum arabic fiber increases fecal nitrogen excretion and lowers serum urea nitrogen concentration in chronic renal failure patients consuming a low-protein diet. Am J Clin Nutr 63:392–39
- ^ Brown RL, Gibson JA, Fenton JC, Snedden W, Clark ML, Sladen GE (1975) Ammonia and urea transport by the excluded human colon. Clin Sci Mol Med 48:279–287
- ^ Skala I, Mareckova O, Ruzickova J, Blaha J, Strakova M, Reneltova I, Jirka J, Kocandrle V, Zvolankova K (1978) Urea and ammonia excretion into gastric juice in regularly dialyzed patients and patients after renal transplantation. I Dialyzed patients. Czech Med 1:180–19020. Havir EA, Tamir H, Ratner S, Warner RC (1965) Biosynthesis of urea XI. Preparation and properties of crystalline argininosuccinase. J Biol Chem 240:3079–3088
- ^ Norifumi Konno 1 , Susumu Hyodo, Kouhei Matsuda, Minoru Uchiyama.Effect of osmotic stress on expression of a putative facilitative urea transporter in the kidney and urinary bladder of the marine toad, Bufo marinus.J Exp Biol.2006 Apr;209(Pt 7):1207-16.
- ^ Luis Marcelo F. Holthauzen, J?rg R?sgen*?, and D. Wayne Bolen*.Hydrogen Bonding Progressively Strengthens upon Transfer of the Protein Urea-Denatured State to Water and Protecting Osmolytes.Biochemistry 2010, 49, 6, 1310–1318.
- ^ Chou C. L., Knepper M. A. (1989). Inhibition of urea transport in inner medullary collecting duct by phloretin and urea analogues. Am. J. Physiol. 257, F359–F365
- ^ Sands J. M. (2002). Molecular approaches to urea transporters. J. Am. Soc. Nephrol. 13, 2795–280610.
- ^ You G., Smith C. P., Kanai Y., Lee W. S., Stelzner M., Hediger M. A. (1993). Cloning and characterization of the vasopressin-regulated urea transporter. Nature 365, 844–84710.
- ^ Buniatian H. C., Davtian M. A. (1966). Urea synthesis in brain. J. Neurochem. 13, 743–75310.
- ^ Couriaud C., Ripoche P., Rousselet G. (1996). Cloning and functional characterization of a rat urea transporter: expression in the brain. Biochim. Biophys. Acta 1309, 197–199
- ^ Lei T., Zhou L., Layton A. T., Zhou H., Zhao X., Bankir L., Yang B. (2011). Role of thin descending limb urea transport in renal urea handling and the urine concentrating mechanism. Am. J. Physiol. Renal Physiol. 301, F1251–F125910.
- ^ Yang B., Bankir L. (2005). Urea and urine concentrating ability: new insights from studies in mice. Am. J. Physiol. Renal Physiol. 288, F881–F89610.
- ^ Lise Bankir, Kai Chen, Baoxue Yang.Lack of UT-B in vasa recta and red blood cells prevents urea-induced improvement of urinary concentrating ability.Am J Physiol Renal Physiol. 2004 Jan;286(1):F144-51.
- ^ Yang B., Bankir L. (2005). Urea and urine concentrating ability: new insights from studies in mice. Am. J. Physiol. Renal Physiol. 288, F881–F89610.
- ^ Lei T., Zhou L., Layton A. T., Zhou H., Zhao X., Bankir L., Yang B. (2011). Role of thin descending limb urea transport in renal urea handling and the urine concentrating mechanism. Am. J. Physiol. Renal Physiol. 301, F1251–F125910.
- ^ Berger U. V., Tsukaguchi H., Hediger M. A. (1998). Distribution of mRNA for the facilitated urea transporter UT3 in the rat nervous system. Anat. Embryol. 197, 405–41410.
- ^ Ferraro PM, Mandel EI, Curhan GC, Gambaro G, Taylor EN (2016) Dietary protein and potassium, diet-dependent net acid load, and risk of incident kidney stones. Clin J Am Soc Nephrol 11:1834–1844











